Idea In Brief
Delivering outcomes
Australian governments have pledged to invest in urgent care services. How can system designers ensure urgent care services deliver the outcomes clinicians, managers and, most crucially, patients, are seeking? From our experience, the crucial factor is how the service is implemented.
Many benefits
We have seen many benefits that urgent care can deliver. These benefits include decreasing the ED burden, shorter wait times, higher patient and staff satisfaction, safe and effective care, comprehensive, convenient care on site, integrated services and cost-effective treatment.
Key questions
We have found there are five key questions for a service designer to consider when developing a model for urgent care: What are the intake pathways?, What is the staffing model?, Where and when should the service operate?, What services should be provided?, What is the funding model?
Everyone knows it. From doctors to hospital administrators, paramedics to nurses, governments to patients, it is clear our hospitals are critically overcrowded. Something needs to be done.
One proposed solution currently getting attention is urgent care – a service to treat non-life threatening urgent medical conditions and accidents.
Australian governments, both national and state, have pledged to invest in urgent care services. But there has been push back from peak bodies who do not feel this will be the solution to the problems plaguing the Australian health system.
While urgent care services alone are unlikely to solve these problems – evident in an ageing population, funding gaps, lack of access to GPs and workforce shortages – they can provide tangible benefits to patients, providers and the healthcare system.
So how can system designers ensure urgent care services deliver the outcomes clinicians, managers and, most crucially, patients, are seeking? From our experience, the crucial factor is the how the service is implemented.
In this article we are pleased to share insights drawn from our experience in urgent care clinic (UCC) review, design and consulting across several states, and through facilitating the first national UCC workshop last year.
We offer five questions – and some guidance on the answers – that can be the difference between a transformational success and a noble failure.
Demand for emergency department and after-hours care is up
To understand the case for urgent care services we need to understand the crisis in emergency departments (ED).
In the year to June 2022, there were 8.8 million presentations at ED, the highest number ever recorded across every state and territory. Over the past five years the increase in ED presentations has exceeded population growth – 14 per cent, compared to 5 per cent.
The rising demand for urgent healthcare services has resulted in worsening ED metrics across Australia, including increased ambulance ramping, longer average wait times to be seen by a health professional and an increased proportion of patients who did not wait for treatment or left the ED at their own risk. The dysfunction resulting from overcrowding risks patient safety.
There is a proportion of ED patients that could be treated elsewhere, such as via urgent care – and the cohort is large enough to sustain urgent care services. If urgent care services are set up right to target and divert these patients, they could alleviate some portion of the ED burden.
This makes these initiatives worthwhile to pursue, but also means they need to be implemented in the right manner to match the target population needs and the referral pathways they utilise.
Urgent care services can benefit healthcare consumers
Urgent care initiatives are popular across the world, including in New Zealand, the United Kingdom, Canada, the United States and the Netherlands.
In Australia, urgent care services have been piloted by all jurisdictions over the past two decades, where models of care differ greatly in their intake pathways, staffing model, service provision, hours, location and funding.
From our work evaluating urgent care services and reviewing research in Australia and abroad, we have seen many benefits that urgent care can deliver:
- Decrease the ED burden. The Royal New Zealand College of Urgent Care (RNZCUC) found that New Zealand cities with urgent care clinics have significantly lower emergency department attendance. In an evaluation of the GP Access After Hours (GPAAH) clinics in New South Wales, 61 per cent of survey respondents said they would have attended an emergency department or called Triple Zero if the service had not been available. Other studies have shown that that as many as 27 per cent of ED visits could be seen at urgent care clinics.
- Shorter wait times. Three evaluations conducted on Australian urgent care services showed wait times to be seen by a provider in urgent care on average to be less than 30 minutes (meanwhile, 90 per cent of patients in Australian EDs were seen within 1 hour and 42 minutes).
- High patient and staff satisfaction. Evaluations and engagement with urgent care providers and patients across Australia have provided overwhelmingly positive feedback. According to Wellbeing SA, 92 per cent of users surveyed were satisfied or very satisfied with the service they received from a priority care service operating in South Australia.
- Safe and effective care. Evaluations have provided evidence of low re-presentation rates, alongside appropriate escalation of patients requiring a higher level of care. The Wellbeing SA study found 96 per cent of patients were discharged home after leaving the priority care service.
- Comprehensive, convenient care on site. Patients are getting the care they need from urgent care services, with little need to refer patients onto other services, including to emergency departments. This care is close to home and has all relevant services in the one place.
- Integrated services. Urgent Care models have integrated with local GPs to provide summaries of patient care, to schedule follow-up for patients and to refer them to outpatient programs such as Hospital in the Home.
- Cost-effective treatment. The cost per patient has been demonstrated by many urgent care initiatives across Australia to be significantly lower than that of an ED visit. An evaluation of GPAAH in NSW showed the cost of services for non-emergent and semi-emergent triage levels to be $132 for GP home visits, $60 for extended-hours GPs, and $53 for in-hours GPs – compared to $402 for ED.
The potential benefits are vast. But how should urgent care services be implemented to realise them?
Be clear on your definition and purpose
The first step in implementing high-impact urgent care is an agreed definition.
Many urgent care-type initiatives have been introduced in Australia under different names – we have seen services branded as “Urgent treatment facilities”, “Urgent care services”, “Priority primary care centres”, “Urgent care clinics”, ‘Priority care centres” and “Urgent treatment centres”. And there are myriad other service offerings that also provide urgent access to care, such as GP after-hours clinics, respiratory clinics, rapid access clinics, home visiting GP services, community pharmacy. The landscape is messy and confusing.
A common definition for what urgent care services will provide relative to other initiatives in the healthcare landscape is important. We believe the definition of urgent care is to provide episodic treatment for non-life threatening urgent medical conditions and accidents in the community.
It is then vital to define the intended outcomes. If you are seeking to reduce the burden on emergency departments, this will lead to a very different service to one that is seeking to fill primary care gaps. The outcome you are seeking will determine how you should operate the urgent care service.
Understand the population needs and urgent care ecosystem
As there are many existing urgent care-type initiatives, it is important the local healthcare landscape is fully understood to guide a new service offering.
To understand the most appropriate services urgent care should offer, system designers need to understand the healthcare ecosystem of a target area. You can see an example of urgent health care ecosystem across Australia here:
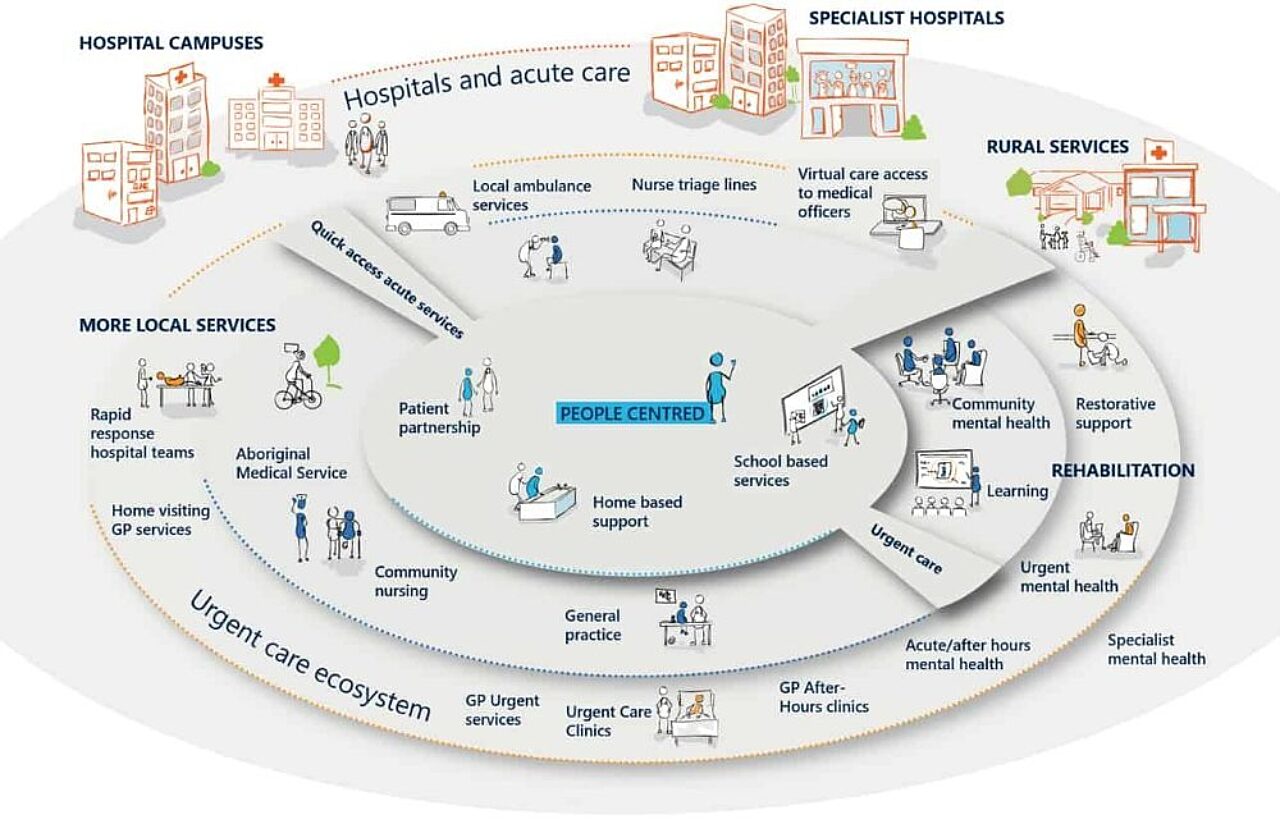
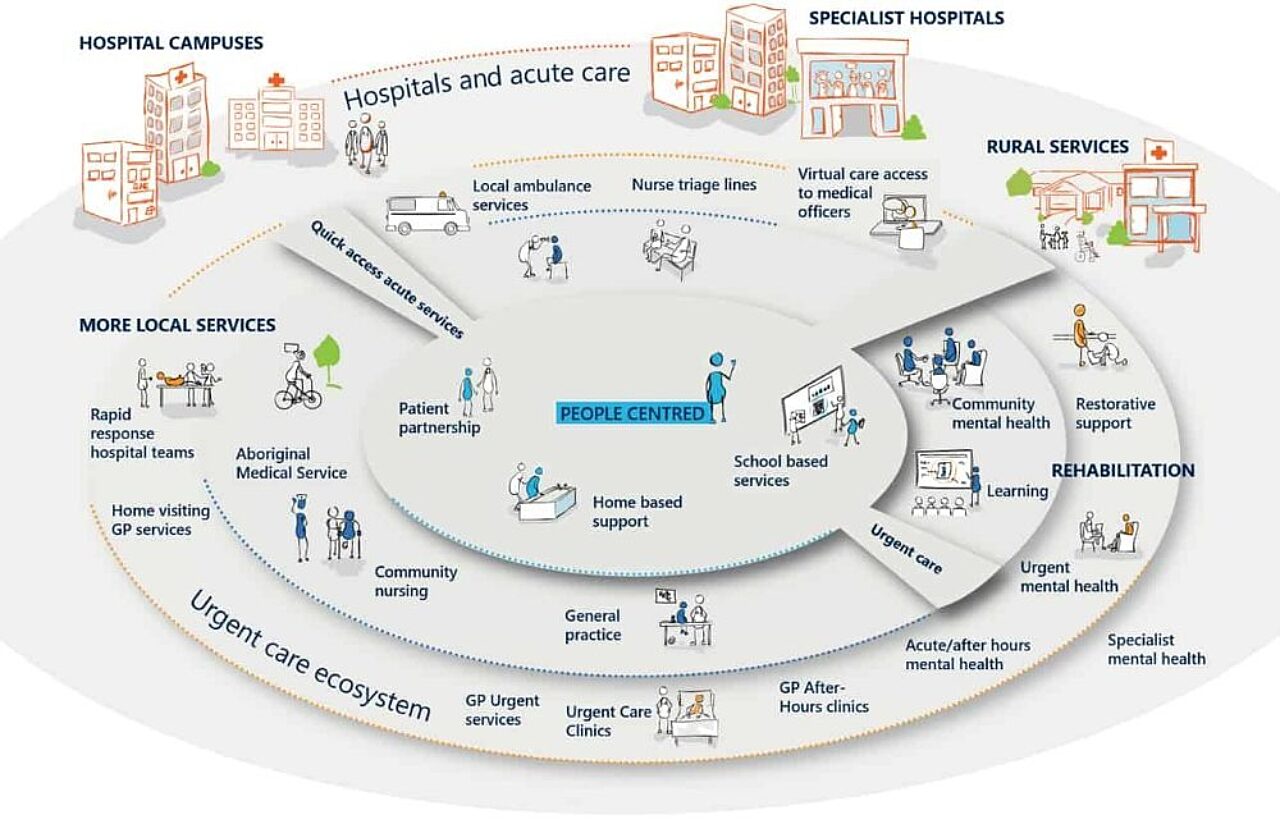
Only by considering the whole ecosystem will an urgent care service integrate with other available services to best meet population health needs. Designers need to understand the types of patients in their region and why they have ended up in ED so they can set up the right diversion models in urgent care.
Urgent care services vary based on community-specific needs and the resources already available to meet those needs. They should not duplicate or complicate an already complex landscape and there is no one-size-fits-all solution.
Convenience and easy navigation should be the key considerations. Taking a person-centred approach and including providers, patients and community members in the process of developing services is essential. And system designers need to make sure all the components are coordinated and connected to make it easy for patients and referrers to navigate to the right place. Community education and campaigning will also be vital.
There are five questions that can make or break an urgent care service
Given this complexity, it is easy for service designers to be overwhelmed by the difficult choices they need to make. While every decision is important, we have found there are five key questions for a service designer to consider when developing a model for urgent care.
Drawing on the experience of experts and others who have tried it before can help guide you to the answer that is right for your context.
There is a window of opportunity to get the model right
When urgent care is integrated with existing services and tailored to population needs, it can improve community health. But get the design wrong, and urgent care services will exacerbate the very problems it is seeking to solve, creating even greater frustration and health system fragmentation.
One jurisdiction leading the way is South Australia. Recently we spoke to Jeanette Walters, a senior health executive with whom we have worked to develop the system. Here’s what she told us:
“Urgent care services need to be developed as an integrated part of the system, not as stand-alone services. Their ability to provide a safe and effective alternative to an emergency department is underpinned by a clear understanding of their scope and good communication pathways with other parts of the system, including emergency departments and general practice.
“Regular feedback and service improvement processes with clinicians, the community and the system more broadly help these services to continue develop in line with local needs and become a trusted and effective part of the system.”
Urgent care services will soon be a part of the urgent healthcare ecosystem in every state and territory. As system designers consider the right model for their community, we encourage them to consider our five key questions.
Get in touch to discuss how we can use our technical expertise to develop high-impact urgent care services.
Connect with Raj Verma on LinkedIn.
Prepared with input from Erika Tait, Kazimier Lim, Paul Eleftheriou and Chris Edwards.

