The National Rural Health Alliance (NRHA) is a peak advocacy body comprising 47 national organisations committed to training the health and medical workforce, delivering health services, and improving the health and wellbeing of the more than 7 million people living in rural, regional and remote Australia.
NRHA needed a baseline of evidence to benchmark and support its advocacy
To accurately monitor the status quo and make its case to the government for a better deal for Australians in rural areas, the NRHA needed to measure the gap in health spending between urban and non-urban areas.
Building this evidence case was no easy task, given the complex mix of public and private health, disability and aged care services in Australia. As a recipient of Nous consulting services through our Community Partnership Scheme, NRHA asked our economics and health specialists to have a go.
We used modelling to compare healthcare use and spending
As a first step, we aligned and analysed public and private data to develop a clear quantitative picture of healthcare use and spending. This data covered a wide breadth of activity, including hospital use, Medicare, the Pharmaceutical Benefits Scheme, the National Disability Insurance Scheme, aged care and dentistry.
The task was made more complicated by the fact that few data sources distributed spending by geographic remoteness. Our solution? Detailed modelling, drawing on other data sources:
- We mapped Census population and postcode data to the Australian Geography Standard Remoteness Area and the Modified Monash Model scale, using mapping data from the Department of Health and elsewhere.
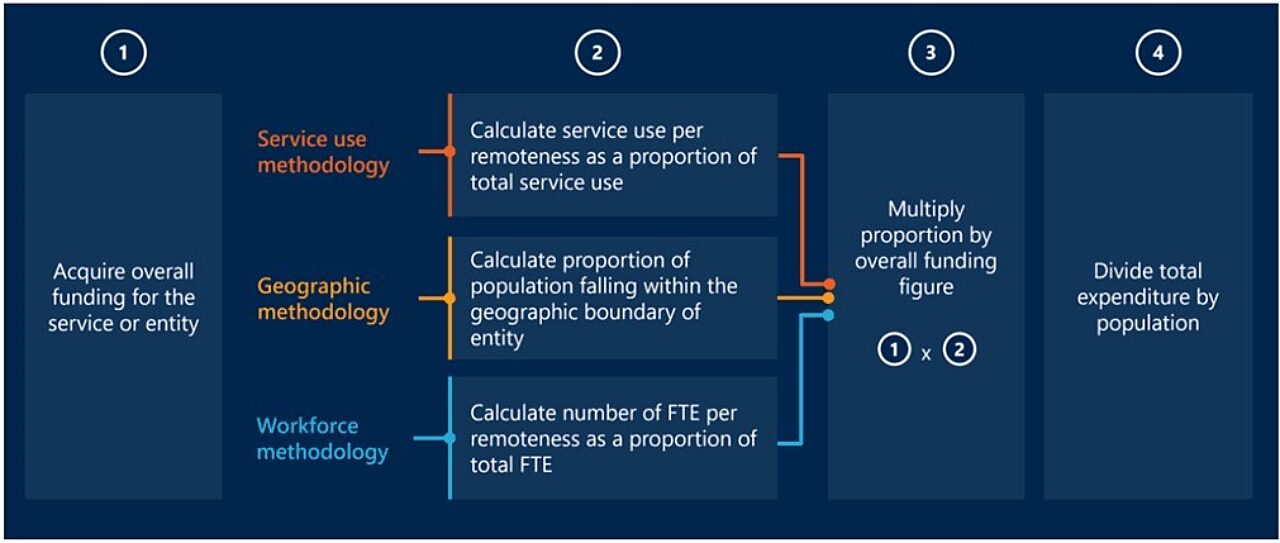
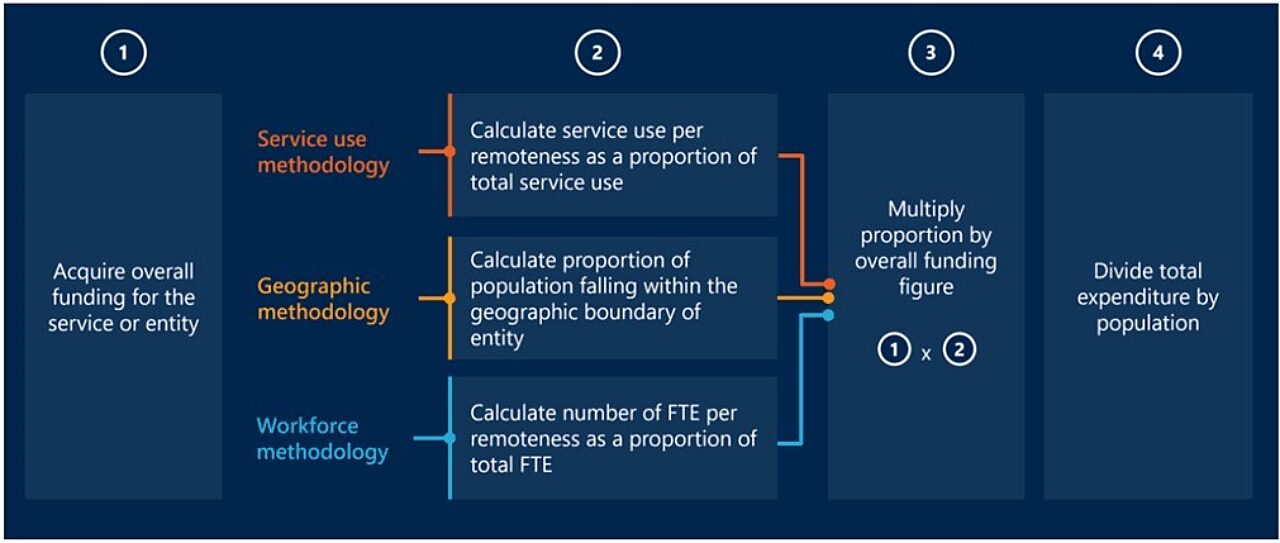
- We used a trio of methods – service-use, geographic and workforce – to determine spending per remoteness.
- We used a geographic method where an entity covered multiple remoteness areas (such as hospital peer groups and primary health networks) and workforce method where neither service use nor geography data was available (such as in the case of dentistry).
- We applied an indirect age standardisation method to control for the effect of differing age distributions on per-person results.
Although crunching the data was useful, it was not enough on its own. So we contextualised our analysis through close collaboration with the client and interviews with key stakeholders in rural health delivery, who provided a comprehensive view.
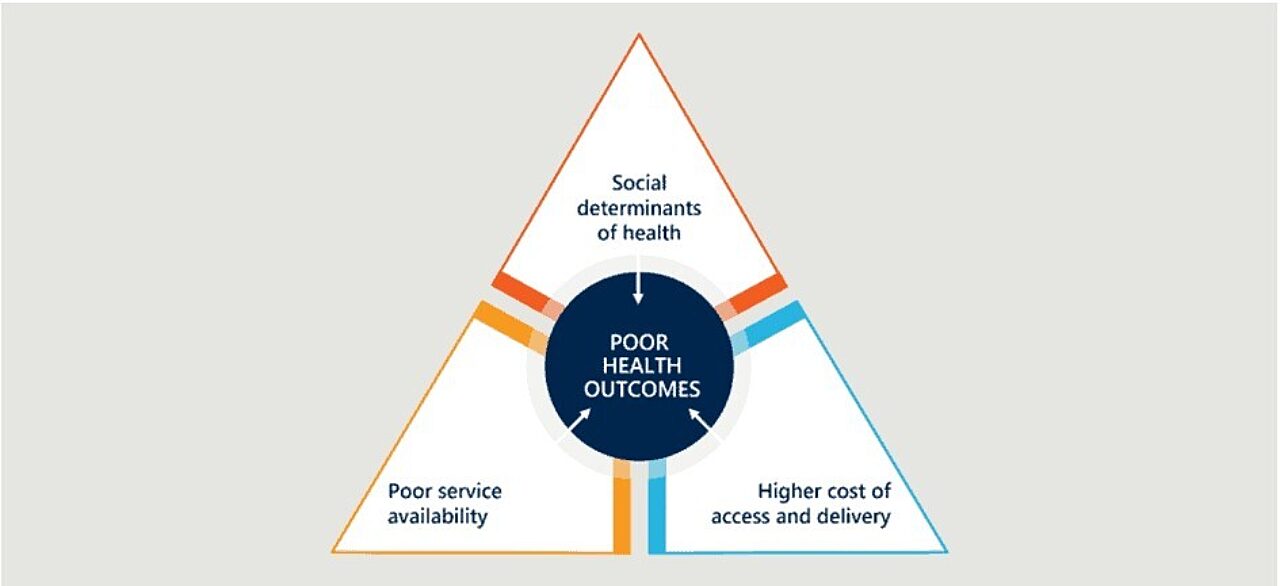
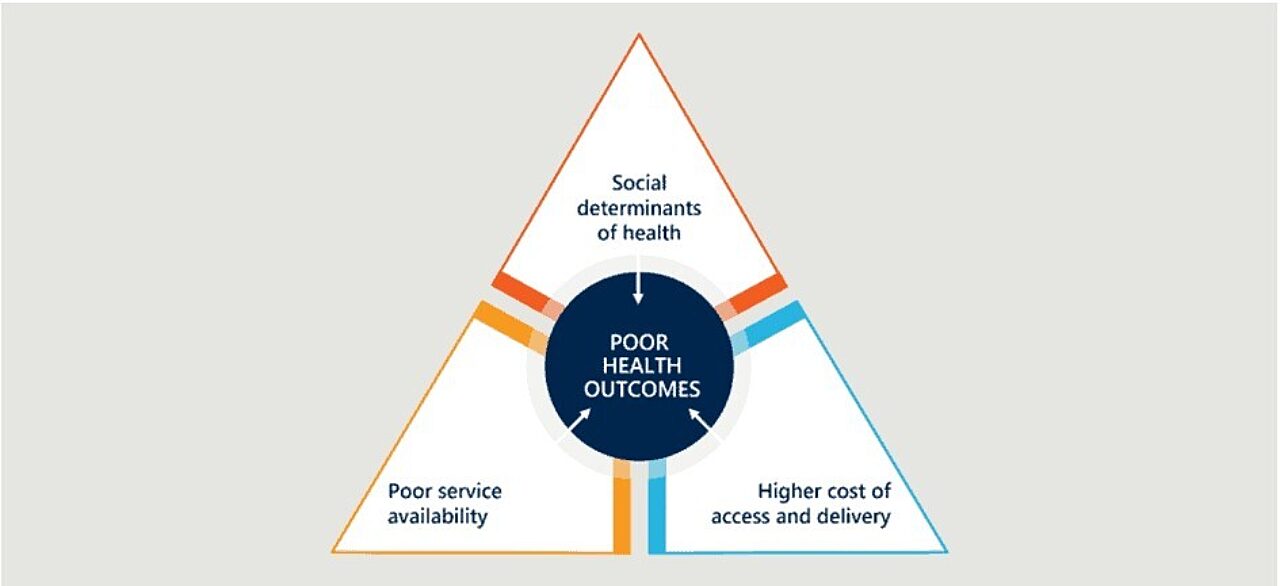
We found alarming spending disparity, backing the case for change
Our report summarises spending shortfalls across multiple health domains for the first time in 10 years. We show that each person in rural Australia is missing out on nearly $850 a year of healthcare access, which equates to a total annual rural health spending deficit of $6.5 billion. The burden of disease in remote areas is 1.4 times that of major cities.
The National Rural Health Alliance released our report (“Evidence base for additional investment in rural health in Australia”), with a supporting media release, in June 2023. The report sparked media interest, including in The Australian, and was welcomed by advocacy groups including the National Farmers Federation, the Australian College of Nurse Practitioners, the Australian College of Rural and Remote Medicine and the Royal Australian College of General Practitioners.
Our findings were presented to the rural health commissioner, Department of Health senior officials, ministers of health and aged care and rural health, and the state minister of health. They have equipped NRHA with powerful data against which to benchmark, and so it can advocate for systemic change in health spending and policy approaches to ensure that expenditure and programs are fit-for-purpose.
What you can learn from this project
When working with limited data, invest time in planning your approach to modelling, data sources and assumptions.
Numbers are more powerful when informed by human experience: supplement quantitative evidence with human insight when possible.
Planning, communication and coordination are key for efficient service utilisation.

